Free Advance Beneficiary Notice of Non-coverage Form
Things You Should Know About This Form
What is the Advance Beneficiary Notice of Non-coverage (ABN)?
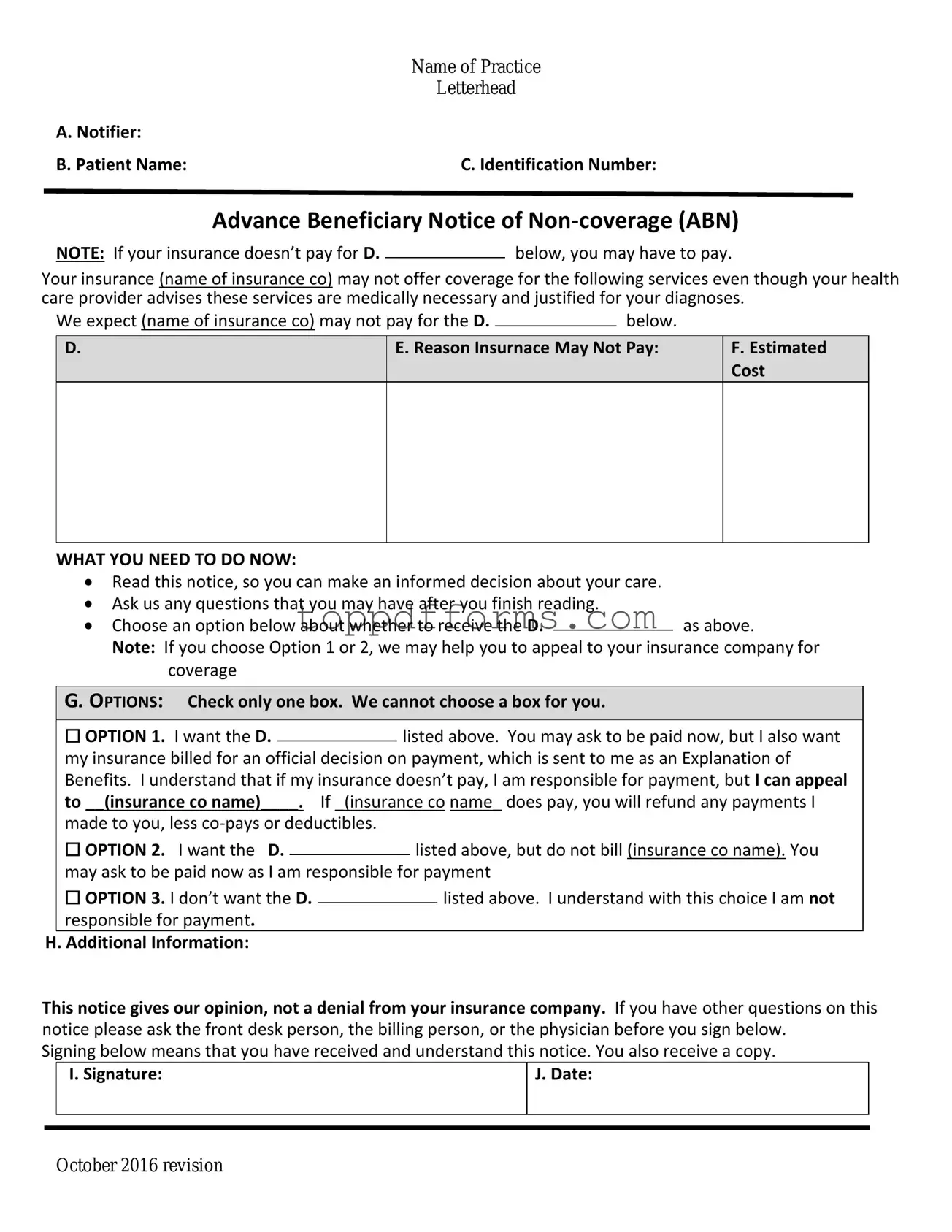
The Advance Beneficiary Notice of Non-coverage, commonly known as the ABN, is a form used by healthcare providers to inform patients that Medicare may not cover a specific service or item. It allows patients to make informed decisions about their care and understand their financial responsibilities before receiving services.
When should I receive an ABN?
You should receive an ABN when a healthcare provider believes that a service or item may not be covered by Medicare. This typically occurs before the service is rendered. The provider must explain why they think Medicare might deny coverage and give you the opportunity to choose whether to proceed with the service.
What happens if I don’t sign the ABN?
If you choose not to sign the ABN, you may still receive the service, but you will be responsible for the costs if Medicare denies coverage. Signing the ABN indicates that you understand the potential for non-coverage and accept the financial responsibility if that occurs.
Do I have to pay for services if I sign the ABN?
Signing the ABN does not automatically mean you will have to pay for the service. It simply acknowledges that you are aware Medicare may not cover it. If Medicare denies the claim, you will be billed for the service. If it is covered, you won’t have to pay anything beyond your usual cost-sharing amounts.
Can I appeal if Medicare denies coverage after I signed the ABN?
Yes, you can appeal Medicare's decision if coverage is denied. The ABN provides you with a clear understanding of the situation, and you can use this information to file an appeal. The process involves submitting a request for reconsideration to Medicare, along with any supporting documentation.
Is the ABN form required for all services?
No, the ABN is not required for every service. It is specifically used when a provider believes that a service may not be covered by Medicare. Some services are always covered, while others may have specific conditions that need to be met for coverage. Your provider will determine if an ABN is necessary based on the service being provided.
What should I do if I don’t understand the ABN?
If you don’t understand the ABN or have questions about it, do not hesitate to ask your healthcare provider for clarification. It’s important to fully understand the implications of signing the form, including your financial responsibilities. Providers are obligated to help you comprehend the information presented.
How long is the ABN valid?
The ABN is valid for the specific service or item it pertains to, and it is only effective for the duration of that service. If you receive a similar service in the future, a new ABN may need to be issued. Each ABN is tied to a particular instance of care, so it’s important to review each one carefully.
What if I don’t agree with the reason for the ABN?
If you disagree with the reason provided for the ABN, you have the right to discuss your concerns with your healthcare provider. They can provide additional information or clarification about why they believe Medicare may not cover the service. If necessary, you can also seek a second opinion from another provider.
Where can I find more information about the ABN?
For more information about the ABN, you can visit the official Medicare website or contact Medicare directly. They provide resources and guidance on understanding the ABN and other Medicare-related topics. Additionally, your healthcare provider should be able to assist you with any questions you may have.
File Information
| Fact Name | Description |
|---|---|
| Purpose | The Advance Beneficiary Notice of Non-coverage (ABN) informs Medicare beneficiaries that a service may not be covered. |
| Who Issues It | Healthcare providers issue the ABN to beneficiaries before providing services that may not be covered by Medicare. |
| When It’s Used | The ABN is used when a provider believes that Medicare may deny payment for a service or item. |
| Beneficiary Rights | Beneficiaries have the right to refuse services after receiving an ABN. |
| State-Specific Forms | Some states may have specific ABN forms governed by local laws. Check state regulations for details. |
| Signature Requirement | Beneficiaries must sign the ABN to acknowledge understanding of potential non-coverage. |
| Impact on Billing | If a service is denied, the provider may bill the beneficiary if they signed the ABN. |
| Validity Period | The ABN is valid only for the specific service or item listed and for the date it was issued. |
Common mistakes
Filling out the Advance Beneficiary Notice of Non-coverage (ABN) form can be a straightforward process, but many people make common mistakes that can lead to confusion and potential issues with Medicare coverage. One frequent error occurs when individuals fail to provide accurate information about the service or item in question. Without clear details, the form may be deemed invalid, leaving beneficiaries uncertain about their financial responsibilities.
Another mistake is neglecting to check the appropriate boxes that indicate whether the service is expected to be covered by Medicare. Beneficiaries often overlook this step, which can result in misunderstandings about what costs they might incur. It is crucial to be diligent in this section to avoid unexpected bills.
Some individuals also forget to sign and date the form. This oversight might seem minor, but it is essential for validating the notice. A missing signature can lead to complications when trying to appeal a decision or clarify coverage. Always remember that your signature is a confirmation of your understanding of the information presented.
Additionally, many people do not take the time to read the instructions thoroughly. The ABN form contains important information that can guide beneficiaries in making informed decisions about their healthcare services. Skipping this step can lead to misunderstandings about the implications of the notice and the potential financial impact.
Lastly, a common mistake is failing to keep a copy of the completed ABN form. Documentation is vital in healthcare matters, and having a record of what was agreed upon can be invaluable in case of disputes or questions regarding coverage. Always ensure that you retain a copy for your records to safeguard your interests.
Popular PDF Forms
Create a Gift Card - A delightful way to show your appreciation!
How Do You Get Pay Stubs If You Are Self Employed - This pay stub format includes important information such as contractor name and payment amount.
Completing a Florida Do Not Resuscitate Order form is an essential step for individuals wishing to clearly communicate their end-of-life preferences. This legally binding document allows patients to state their desire to forgo cardiopulmonary resuscitation (CPR) in emergency situations, ensuring that their wishes are honored by medical professionals. It is particularly relevant for those facing serious health conditions, and more information about the form can be found at https://floridaformspdf.com/printable-do-not-resuscitate-order-form.
Konami Decklist - Maintain neatness in your handwriting to facilitate a smooth process.