Free Do Not Resuscitate Order Template
State-specific Guidelines for Do Not Resuscitate Order Documents
Things You Should Know About This Form
What is a Do Not Resuscitate (DNR) Order?
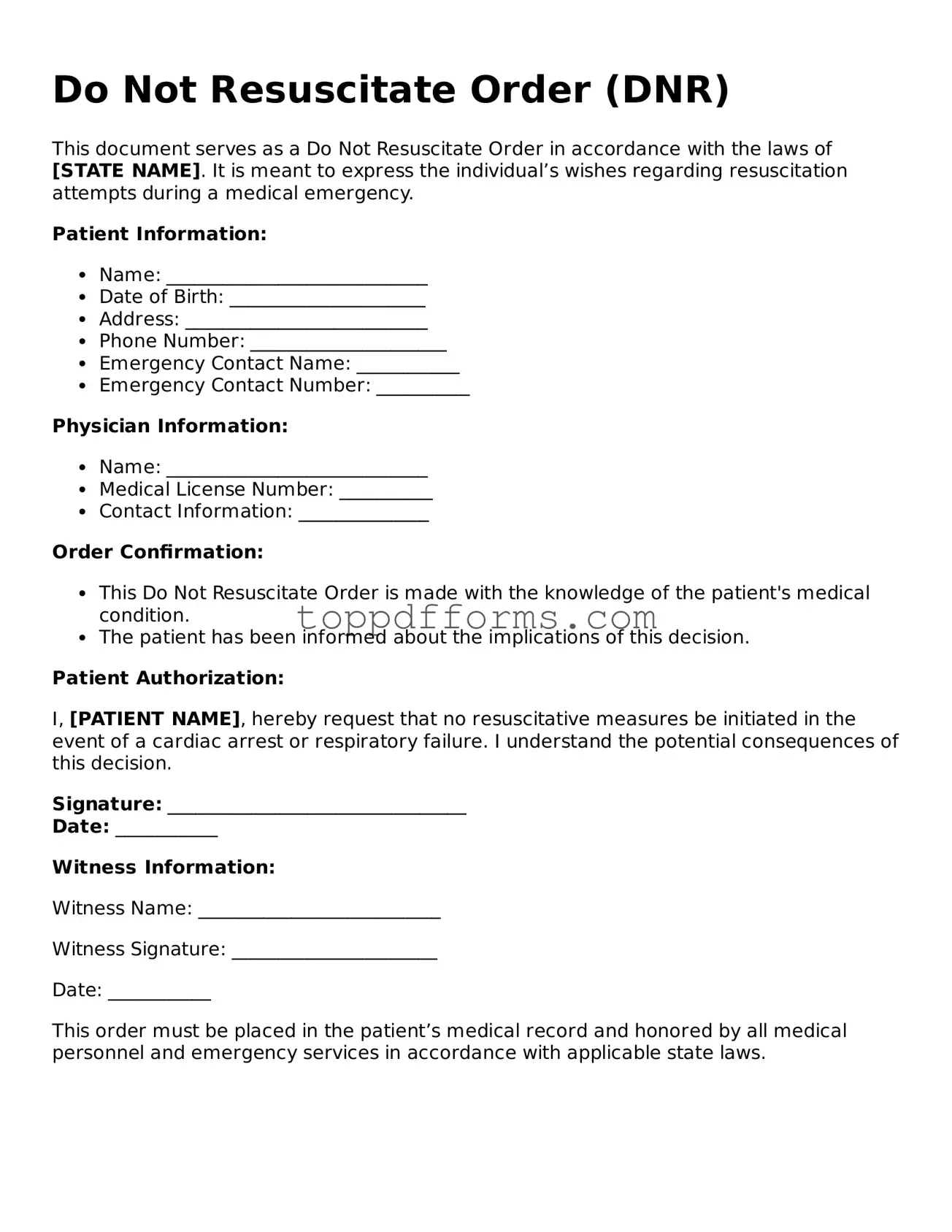
A Do Not Resuscitate Order is a legal document that allows individuals to refuse certain life-saving medical interventions, specifically cardiopulmonary resuscitation (CPR), in the event of cardiac arrest or respiratory failure. This order is intended for patients who have a terminal illness, are in a persistent vegetative state, or have a serious medical condition where resuscitation would not improve their quality of life. The DNR order must be signed by a physician and is usually placed in the patient's medical record.
Who can request a DNR Order?
Typically, the patient themselves can request a DNR order if they are mentally competent. In cases where the patient is unable to communicate their wishes, a legal representative, such as a family member or a designated healthcare proxy, may be able to request the order on their behalf. It is important that the individual requesting the DNR fully understands the implications of the order and that it reflects the patient’s wishes.
How is a DNR Order implemented in a healthcare setting?
Once a DNR order is signed by the physician and the patient or their representative, it becomes part of the patient’s medical record. Healthcare providers are then required to follow the order in emergency situations. It is crucial for the DNR order to be clearly documented and accessible to all members of the healthcare team to ensure that the patient's wishes are respected during medical emergencies.
Can a DNR Order be revoked?
Yes, a DNR order can be revoked at any time by the patient or their legal representative. This can be done verbally or in writing. It is advisable to inform the healthcare team and ensure that the medical records are updated accordingly. If the DNR order is no longer desired, healthcare providers must be made aware to prevent any confusion during emergencies.
What should individuals consider before signing a DNR Order?
Before signing a DNR order, individuals should carefully consider their medical condition, prognosis, and personal values regarding end-of-life care. Discussions with healthcare providers, family members, and legal advisors can provide clarity and help individuals make informed decisions. It is important to understand that a DNR order does not affect other types of medical treatment and that patients can still receive comfort care and pain management.
PDF Overview
| Fact Name | Description |
|---|---|
| Definition | A Do Not Resuscitate (DNR) Order is a legal document that instructs medical personnel not to perform cardiopulmonary resuscitation (CPR) in the event of cardiac arrest. |
| Governing Law | Each state has specific laws governing DNR orders. For example, in California, the DNR is governed by the California Health and Safety Code Section 7180-7184. |
| Patient Autonomy | DNR orders respect the wishes of patients regarding their end-of-life care, allowing them to make decisions about their treatment preferences. |
| Healthcare Provider Obligations | Healthcare providers are required to honor valid DNR orders as part of their ethical and legal responsibilities to patients. |
| State-Specific Forms | Many states provide specific forms for DNR orders, which must be completed and signed by the patient or their authorized representative. |
| Emergency Situations | In emergency situations, medical personnel must verify the existence of a DNR order before withholding resuscitation efforts. |
Common mistakes
Filling out a Do Not Resuscitate (DNR) Order form is a critical decision that requires careful consideration. However, many individuals make common mistakes that can lead to confusion or unintended consequences. Understanding these pitfalls can help ensure that your wishes are accurately documented.
One frequent mistake is failing to sign the form. A DNR order is not valid without the appropriate signatures. Both the patient and the physician must sign the document. Without these signatures, healthcare providers may not honor the DNR wishes.
Another error involves not discussing the DNR order with family members. Open communication is essential. Family members should understand the patient's wishes to prevent misunderstandings during a medical emergency. Without this discussion, loved ones may feel conflicted about the decision.
Some people mistakenly select the wrong options on the form. It's important to read each section carefully. Misunderstanding the choices available can lead to unintended outcomes. For instance, some may think they are opting for a DNR when they are actually consenting to aggressive treatment.
Additionally, individuals often forget to update the DNR order. Life circumstances can change, and so can a person's wishes. If a patient’s health status changes or they have a change of heart, the DNR order should be revised accordingly.
Another common mistake is using outdated forms. Regulations and guidelines can evolve. Always ensure that you are using the most current version of the DNR order form specific to your state. Using an outdated form may cause legal complications.
Some individuals neglect to provide copies of the DNR order to relevant parties. It is essential to share copies with healthcare providers, family members, and anyone involved in the patient's care. Without these copies, the DNR wishes may not be honored in a medical setting.
Inaccurate information can also be a problem. Filling out the form with incorrect personal details, such as the patient's name or date of birth, can lead to legal issues. Ensure that all information is accurate and up-to-date to avoid complications.
Another mistake is not considering state-specific laws. Each state has its own regulations regarding DNR orders. Familiarize yourself with local laws to ensure compliance and validity. Ignoring these laws can result in the DNR order being disregarded.
Lastly, some people may not fully understand the implications of a DNR order. It is crucial to comprehend what a DNR means for treatment options and end-of-life care. Consulting with a healthcare professional can provide clarity and help make informed decisions.
Common Documents
Puppy Health Record - Include names of the sire and dam for lineage tracking.
When engaging in the sale or purchase of a trailer, understanding the importance of the Trailer Bill of Sale is crucial. This document serves to legally confirm the transfer of ownership and includes key details such as specifications, sale price, and the involved parties' identities. For assistance in creating this necessary document, you can find useful templates at PDF Templates.
Pharmacy Medication Labels - Line specifying how often the medication should be taken.